Understanding Carotid Artery Stenosis
Carotid artery stenosis, a condition characterized by the narrowing of the carotid arteries, is a significant contributor to strokes. These arteries, located on each side of your neck, supply blood to your brain. When they become narrowed or blocked, the risk of stroke increases dramatically. Understanding the causes, symptoms, and treatment options for carotid artery stenosis is crucial for managing and preventing this potentially life-threatening condition.
This guide delves into the different causes, symptoms, as well as treatment options for Carotid Artery Stenosis so that when the situation arises, you are well-equipped with the necessary information to deal with the situation.
What is Carotid Artery Stenosis?
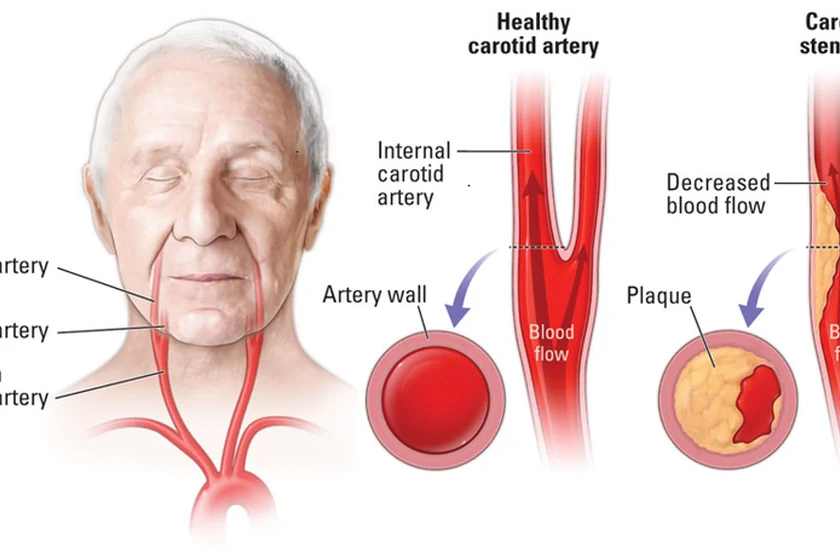
Carotid artery stenosis refers to the narrowing of the carotid arteries due to the buildup of plaque—a mixture of fat, cholesterol, and other substances. This condition is a form of atherosclerosis, where arteries become hardened and narrowed.
Over time, plaque accumulation can significantly restrict blood flow to the brain, leading to an increased risk of ischemic strokes.
Approximately 10-20% of strokes are attributed to carotid artery stenosis, making it a critical area of focus for cardiovascular health.
What are the Causes of Carotid Artery Stenosis?
Carotid artery stenosis develops due to several interrelated factors that contribute to the narrowing of the carotid arteries. Understanding these causes is crucial for both prevention and management of the condition.
Atherosclerosis
The primary cause of carotid artery stenosis is atherosclerosis. This condition involves the buildup of fatty deposits, known as plaques, on the inner walls of the arteries. Plaques are composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin (a clotting material in the blood).
Over time, these plaques harden and narrow the arteries, restricting blood flow. The process begins with damage to the endothelium, the inner lining of the artery, often caused by high blood pressure, smoking, or high cholesterol. This damage allows cholesterol and other substances to penetrate the arterial wall, leading to plaque formation. As plaques grow, they can significantly reduce or block blood flow to the brain, increasing the risk of stroke.
High Blood Pressure
Hypertension, or high blood pressure, is a major risk factor for carotid artery stenosis. Elevated blood pressure can cause damage to the endothelial cells lining the arteries, making them more prone to plaque accumulation. The constant pressure exerted by high blood pressure strains the artery walls, leading to tears and microscopic injuries.
These injuries become sites where plaques can easily form and grow, further narrowing the arteries. Managing blood pressure through lifestyle changes and medication is crucial to reducing the risk of atherosclerosis and carotid artery stenosis.
High Cholesterol Levels
High levels of cholesterol, particularly low-density lipoprotein (LDL) cholesterol, contribute significantly to the development of atherosclerosis and carotid artery stenosis. LDL cholesterol, often referred to as “bad” cholesterol, can infiltrate the damaged areas of the arterial walls and form plaques. Over time, these plaques harden and narrow the arteries, restricting blood flow.
Conversely, high-density lipoprotein (HDL) cholesterol, known as “good” cholesterol, helps remove LDL cholesterol from the bloodstream, reducing the risk of plaque formation. Maintaining a healthy cholesterol balance through diet, exercise, and medications can help prevent carotid artery stenosis.
Smoking
Smoking is a well-established risk factor for atherosclerosis and carotid artery stenosis. The chemicals in tobacco smoke damage the endothelium, making the arteries more susceptible to plaque buildup. Smoking also increases the levels of LDL cholesterol and decreases HDL cholesterol, further contributing to plaque formation.
Additionally, nicotine and other chemicals in tobacco smoke promote inflammation and blood clotting, which can exacerbate the narrowing of the arteries. Quitting smoking is one of the most effective measures to reduce the risk of carotid artery stenosis and other cardiovascular diseases.
Diabetes
Diabetes is another significant risk factor for carotid artery stenosis. High blood sugar levels associated with diabetes can damage the blood vessels and accelerate the process of atherosclerosis. Diabetic individuals often have higher levels of LDL cholesterol and lower levels of HDL cholesterol, increasing the likelihood of plaque formation.
Moreover, diabetes can cause chronic inflammation, which further damages the arterial walls and promotes plaque buildup. Managing blood sugar levels through diet, exercise, and medication is essential for preventing the progression of carotid artery stenosis in diabetic patients.
Age and Family History
Age and genetic factors also play a crucial role in the development of carotid artery stenosis. As people age, the risk of atherosclerosis and carotid artery stenosis increases. The arteries naturally become less flexible and more prone to damage, making them more susceptible to plaque buildup.
Additionally, a family history of atherosclerosis, cardiovascular disease, or stroke can increase an individual’s risk of developing carotid artery stenosis. Genetic predisposition to high cholesterol levels, hypertension, and other related conditions can also contribute to the development of the disease.
Symptoms of Carotid Artery Stenosis
Carotid artery stenosis often progresses silently, especially in its early stages, making it challenging to detect without medical screening. However, as the narrowing of the carotid arteries becomes more pronounced, several symptoms may manifest, indicating reduced blood flow to the brain. Recognizing these symptoms is crucial for early diagnosis and prevention of severe complications like stroke.
Transient Ischemic Attacks (TIAs)
TIAs, also known as mini-strokes, are temporary episodes of stroke-like symptoms that resolve within minutes to hours. They serve as critical warning signs of a potential full-blown stroke.
Common symptoms of TIAs include:
- Sudden Weakness or Numbness: Typically affects one side of the body, often the face, arm, or leg.
- Difficulty Speaking: Slurred speech or inability to find the right words.
- Vision Problems: Sudden vision loss or blurred vision in one or both eyes.
- Dizziness and Loss of Balance: Sudden trouble walking, loss of coordination, or unexplained falls.
- Confusion: Sudden difficulty understanding others or forming coherent sentences.
Stroke
A stroke occurs when blood flow to part of the brain is significantly reduced or blocked, leading to brain cell damage. Symptoms of a stroke are similar to those of a TIA but more severe and longer-lasting. They include:
- Severe Headache: Sudden, intense headache with no known cause, sometimes accompanied by vomiting or altered consciousness.
- Sudden Confusion: Difficulty understanding speech or sudden trouble speaking.
- Sudden Vision Changes: Loss of vision in one or both eyes or double vision.
- Sudden Dizziness: Loss of balance, coordination issues, or trouble walking.
- Paralysis or Numbness: Sudden numbness or weakness in the face, arm, or leg, particularly on one side of the body.
Bruit
A bruit is a whooshing sound heard over the carotid artery during a physical examination with a stethoscope. This sound indicates turbulent blood flow due to the narrowing of the artery. While not a symptom felt by the patient, it is a significant clinical finding that can prompt further investigation.
Cognitive Impairment
In some cases, reduced blood flow to the brain over time can lead to subtle cognitive changes, including:
- Memory Problems: Difficulty remembering recent events or information.
- Difficulty Concentrating: Trouble focusing on tasks or maintaining attention.
- Mental Fatigue: Feeling mentally exhausted more quickly than usual.
Fatigue and General Weakness
Although less specific, chronic fatigue and general weakness can be associated with reduced blood flow and oxygen delivery to the brain and other tissues.
Facial Drooping
One side of the face may droop or become numb. This is often noticeable when the person smiles, as the smile may appear uneven.
Diagnosing Carotid Artery Stenosis
Diagnosing carotid artery stenosis involves several steps and tests:
- Physical Examination: A healthcare provider may listen for a bruit in the neck using a stethoscope.
- Ultrasound or Carotid Doppler: Carotid ultrasound is a non-invasive test that uses sound waves to create images of the carotid arteries and detect blockages.
- CT Angiography (CTA): This imaging test provides detailed pictures of the blood vessels and can identify the extent of narrowing.
- Magnetic Resonance Angiography (MRA): MRA uses magnetic fields and radio waves to produce detailed images of blood vessels.
- Cerebral Angiography or Digital Subtraction Angiography (DSA): This invasive procedure involves injecting a contrast dye into the blood vessels and taking X-rays to visualize blockages.
Treatment Options for Carotid Artery Stenosis
Treatment for carotid artery stenosis aims to reduce the risk of stroke and involves both medical and surgical approaches:
- Lifestyle Changes: Adopting a healthy lifestyle is crucial. This includes quitting smoking, maintaining a healthy diet, exercising regularly, and controlling blood pressure and cholesterol levels.
- Medications: Antiplatelet medications (e.g., aspirin) and anticoagulants (e.g., warfarin) can help prevent blood clots. Statins may be prescribed to lower cholesterol levels.
- Carotid Endarterectomy: A surgical procedure where a surgeon removes plaque from the carotid artery. It is recommended for individuals with significant blockage of more than 70% and symptoms.
- Carotid Artery Stenting: This minimally invasive procedure involves placing a stent (a small mesh tube) to widen the narrowed artery and improve blood flow. This can be achieved under local anesthesia via a small needle puncture in the groin.
Prevention of Carotid Artery Stenosis
Preventing carotid artery stenosis involves managing risk factors and making healthy lifestyle choices:
- Healthy Diet: Consuming a diet rich in fruits, vegetables, whole grains, and lean proteins while limiting saturated fats and cholesterol.
- Regular Exercise: Engaging in regular physical activity helps maintain healthy blood pressure and cholesterol levels.
- Smoking Cessation: Quitting smoking significantly reduces the risk of atherosclerosis and subsequent carotid artery stenosis.
- Blood Pressure and Cholesterol Management: Regular monitoring and control of blood pressure and cholesterol levels through medication and lifestyle changes.
- Regular Check-Ups: Routine medical check-ups can help detect early signs of atherosclerosis and other cardiovascular issues.
Conclusion
Carotid artery stenosis is a serious condition that can significantly increase the risk of stroke if left untreated. Understanding the causes, recognizing the symptoms, and being aware of the various treatment options are crucial steps in managing this condition effectively. Regular check-ups and early diagnosis play vital roles in preventing severe complications. If you or someone you know is experiencing symptoms related to carotid artery stenosis, it is essential to seek medical advice promptly.
For those looking for specialized care, consulting with a vein specialist doctor near me can provide tailored treatment options and expert guidance. Dr. Sumit Kapadia, a renowned specialist in vascular and endovascular surgery, offers comprehensive care for carotid artery disease and related conditions. With his extensive experience and dedication to patient health, Dr. Kapadia is committed to providing the highest standard of care. Do not hesitate to schedule a consultation to explore the best treatment options for maintaining your vascular health.
FAQs
The best treatment for carotid artery stenosis depends on the severity of the blockage and individual patient factors, but options include medication, lifestyle changes, endovascular procedures like carotid angioplasty and stenting, or surgical intervention such as carotid endarterectomy.
First signs of a blocked carotid artery may include transient ischemic attacks (TIAs), and stroke-like symptoms that resolve within minutes to hours, such as sudden weakness or numbness on one side of the body, difficulty speaking, vision problems, dizziness, or confusion. Often, these blockages can often be asymptomatic and are detected on Doppler evaluation.
Medicine alone may not cure 90% blockage of the carotid artery, but it can help manage symptoms and reduce the risk of stroke. Treatment options may include antiplatelet medications, anticoagulants, statins, blood pressure medications, and lifestyle modifications.
To naturally unblock the carotid artery, focus on adopting a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, regular exercise, maintaining a healthy weight, quitting smoking, managing stress, and controlling other risk factors such as high blood pressure, high cholesterol, and diabetes.
The first-line treatment for carotid stenosis typically involves antiplatelet agents like aspirin or clopidogrel, along with statins to lower cholesterol levels. In severe cases or high-risk situations, carotid endarterectomy or carotid artery stenting may be considered.




