Carotid artery disease is one of the leading causes of preventable stroke. As a vascular surgeon, I often meet patients who are surprised to learn that their risk of stroke is linked to a narrowing in the arteries of the neck.
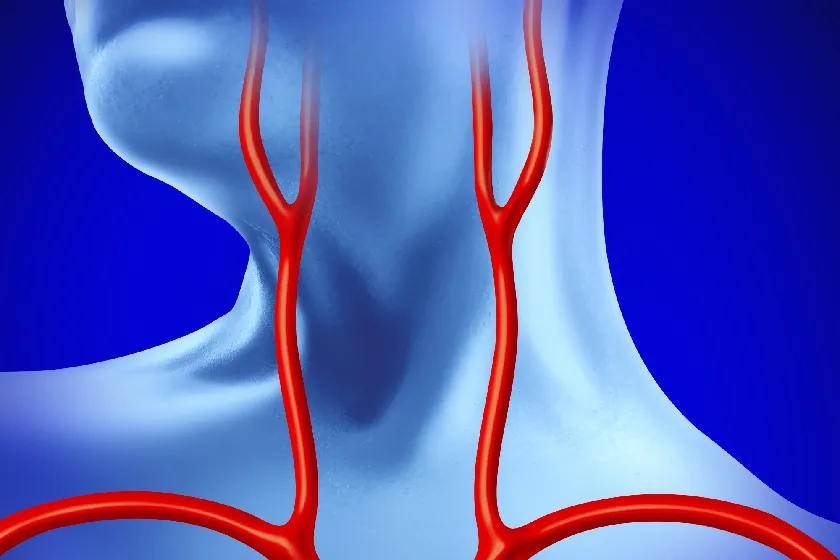
These arteries, known as the carotid arteries, supply oxygen-rich blood to the brain. When they become blocked or narrowed due to plaque build-up, the brain’s blood supply is compromised, which can lead to a stroke.
The decision to undergo surgery depends on multiple factors, but when done at the right time, it can prevent life-threatening events and preserve quality of life.
What is Carotid Disease?
Carotid artery disease occurs when fatty deposits (plaque) made of cholesterol, calcium, and other substances accumulate inside the carotid arteries. Over time, this build-up causes the arteries to harden and narrow, a condition called atherosclerosis.
When the narrowing becomes severe, blood flow to the brain is reduced, or a clot may form and travel to the brain, causing a stroke or a transient ischemic attack (TIA), often called a mini-stroke. The condition is more common in older adults, but risk factors such as smoking, high blood pressure, diabetes, high cholesterol, and a sedentary lifestyle can accelerate its development.
Key Factors in the Decision for Surgery
Symptomatic Patients (>70% Blockage)
If a patient has experienced warning signs of stroke, such as sudden weakness or numbness in the face or limbs, difficulty speaking, vision changes, or loss of balance, and tests show more than 70 percent narrowing of the carotid artery, surgery is strongly recommended.
At this stage, the risk of a major stroke is high, and surgical intervention like carotid endarterectomy or stenting can significantly reduce that risk. In my experience, timely surgery in such patients can mean the difference between returning to normal life and facing permanent disability.
Asymptomatic Patients (>80% Blockage)
Some patients have no symptoms, but ultrasound or CT angiography reveals significant narrowing. If the blockage is more than 80 percent and the patient has additional risk factors like heart disease, uncontrolled diabetes, or a history of smoking, surgery may be advised to prevent future strokes.
This is especially true for younger patients with a long life expectancy, as their risk of developing symptoms or having a stroke increases over time. The decision is made after carefully weighing surgical benefits against possible risks.
Degree of Stenosis
The percentage of narrowing, known as the degree of stenosis, plays a central role in decision-making. Mild narrowing (less than 50 percent) is generally managed with medicines and lifestyle modifications. Moderate narrowing (50–69 percent) requires regular monitoring and may need surgery if symptoms appear. Severe narrowing (70 percent or more) almost always needs surgical correction in symptomatic patients, and often in selected asymptomatic patients too.
Surgical Risk Assessment
Before recommending surgery, I conduct a thorough evaluation of the patient’s heart, lungs, kidneys, and overall medical condition.
For example, a patient with uncontrolled heart disease may need cardiac optimization before carotid surgery. The surgical risk assessment ensures that the procedure is both safe and beneficial. It also helps determine whether the patient would be better suited for open surgery or a minimally invasive stenting approach.
Alternative Treatments
Not every patient with carotid artery disease is an immediate candidate for surgery. In those with mild narrowing or high surgical risk, we focus on aggressive medical management – controlling blood pressure, lowering cholesterol, managing diabetes, prescribing antiplatelet medicines, and recommending regular physical activity.
Quitting smoking is critical, as it can significantly slow disease progression. Such patients are closely monitored with regular Doppler ultrasounds to detect any changes that might require surgical intervention in the future.
Surgical Options
Carotid Endarterectomy (CEA)
This is considered the gold standard for treating significant carotid artery narrowing. In this procedure, I make an incision in the neck to access the artery, open it, and carefully remove the plaque, along with a layer of the media of the artery, using specialised instruments.
The artery is then repaired, usually with a patch, to restore smooth blood flow. CEA has been extensively studied and has proven to greatly reduce the risk of stroke in suitable patients.
Carotid Artery Stenting (CAS)
For patients who are not good candidates for open surgery due to anatomy or other medical conditions, carotid artery stenting offers a less invasive alternative. A small tube called a stent is placed inside the artery via a catheter inserted through the groin or wrist. While doing carotid angioplasty, most vascular surgeons would also use a filter device to prevent any small particles from moving to the brain during balloon dilation.
The stent keeps the artery open, maintaining blood flow. While recovery is usually quicker, the choice between CEA and CAS depends on multiple factors, including plaque characteristics and patient health.
Making the Decision
Choosing the right treatment requires a personalised approach. I consider the degree of narrowing, whether symptoms are present, patient age, overall health, and lifestyle.
I also involve the patient and family in every step of the decision-making process so they clearly understand the benefits, risks, and expected recovery. Surgery is not the right choice for everyone, but for those who meet the criteria, it can be life-saving.
Conclusion
Carotid artery disease is a silent yet serious condition that can suddenly cause a stroke if ignored. Recognising when surgery is needed and acting at the right time is critical. With timely diagnosis, expert surgical care, and a tailored treatment plan, the chances of preventing a stroke improve significantly.
If you have been diagnosed with carotid artery narrowing, consult an experienced vascular surgeon who specialises in carotid artery disease surgery.
Frequently Asked Questions
Surgery is recommended for patients with more than 70 percent blockage who have symptoms, or selected asymptomatic patients with more than 80 percent blockage and high stroke risk.
Generally, a blockage above 70 percent in symptomatic patients requires surgery. In certain high-risk cases, more than 80 percent narrowing may also require surgical correction.
Yes. In symptomatic patients, a 70 percent narrowing significantly increases stroke risk, and surgery can substantially reduce this risk.
Most patients undergoing carotid artery surgery are above 60 years old, though younger patients with severe narrowing and risk factors may also require the procedure.

Dr. Sumit Kapadia
MBBS, MS, MRCS, DNB-Fellow



