Over the years, I have met many patients who visit me with complaints like cramping in the legs while walking, cold feet, or slow-healing wounds. Most of them are unaware that these could be signs of Peripheral Vascular Disease, also known as PVD.
Peripheral Vascular Disease is a condition that affects the arteries outside the heart and brain. It often begins silently and gradually worsens, especially if not addressed in time. The good news is that it is both preventable and treatable.
In this article, I aim to help you understand what Peripheral Vascular Disease is, what symptoms to watch out for, what causes it, and most importantly, how it can be treated effectively.
What Is Peripheral Vascular Disease (PVD)
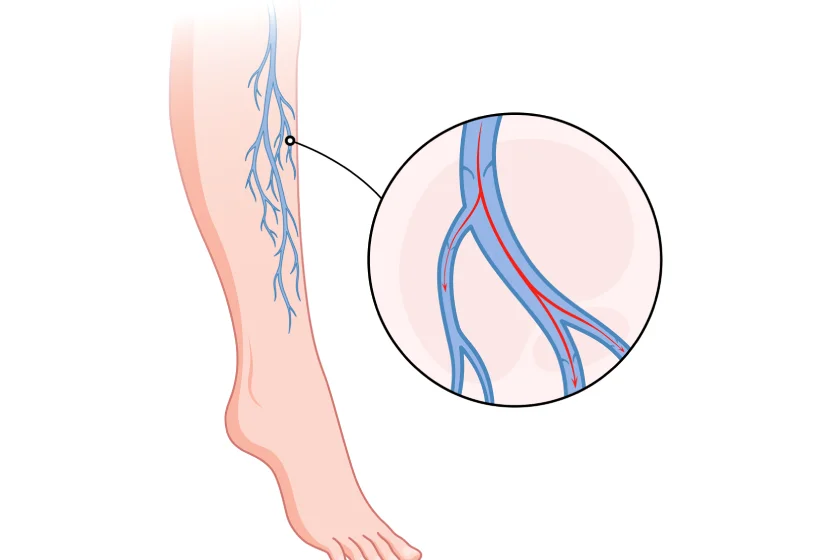
Peripheral Vascular Disease refers to the narrowing or blockage of blood vessels, typically arteries, that supply the legs, arms, stomach, or kidneys. Most commonly, it affects the arteries of the legs and is also referred to as Arterial Peripheral Vascular Disease.
When blood flow is reduced, the muscles and tissues do not receive enough oxygen. This leads to symptoms such as pain while walking or standing, and in severe cases, ulcers or gangrene.
Many people confuse PVD with PAD, or Peripheral Artery Disease. While they are often used interchangeably, PAD specifically refers to arterial blockages, while PVD is a broader term that may also include venous issues.
Peripheral Vascular Disease Symptoms
The most common PVD symptoms include:
- Leg pain or cramping while walking or climbing stairs, also called claudication
- Numbness or weakness in the legs
- Cold feet or legs, especially compared to the other side
- Sores or ulcers on the legs or feet that do not heal
- Weak or absent pulse in the legs
- Shiny skin or loss of hair on the legs and feet
- Discoloration of the skin or blackened toes in advanced stages
Symptoms may be subtle in the beginning but tend to worsen over time if the underlying cause is not treated.
Peripheral Vascular Disease Causes
There are several known causes of Peripheral Vascular Disease. The most common is atherosclerosis, a condition in which fatty deposits build up inside the arteries and reduce blood flow.
Other causes include:
- Smoking, which directly damages the arteries
- Diabetes, which accelerates arterial disease
- High cholesterol and high blood pressure
- Obesity and a sedentary lifestyle
- Inflammatory conditions affecting the blood vessels (For e.g., Buerger’s disease)
- Genetic predisposition (hypercoagulable states or thrombophilia)
Early diagnosis is critical because untreated PVD can lead to serious complications such as non-healing wounds, infections, and even amputation.
Peripheral Vascular Disease Treatment Options
Fortunately, treatment for PVD is available and can be highly effective when started early. The treatment plan usually depends on the severity of the disease and the patient’s overall health.
- Lifestyle changes
Quitting smoking, regular walking, and a balanced diet are the first steps in controlling PVD. Exercise improves blood flow and helps relieve symptoms. In fact, supervised walking programs are often recommended as part of treatment. - Medications
Certain medications may be prescribed to improve blood flow, reduce cholesterol, or manage blood pressure and diabetes. Antiplatelet drugs such as aspirin or clopidogrel can also help prevent clots. - Minimally invasive procedures
In cases where blockages are significant, we may consider angioplasty or stenting. These are image-guided procedures that open up narrowed arteries using a balloon or stent, often performed under local anesthesia. - Surgical treatment
For more advanced disease or long blockages, surgical bypass may be required. In this procedure, a healthy blood vessel is used to bypass the blocked segment.
Every patient is different, and treatment is customized based on the severity of the disease, lifestyle, and individual preferences.
When to See a Vascular Specialist
You should consult a vascular surgeon if you experience:
- Pain in the legs while walking
- Cold or numb feet
- Non-healing ulcers or wounds
- Skin changes such as discoloration or thinning
These are not just signs of aging. They could be signs of Peripheral Arterial Disease or other forms of Peripheral Vascular Disease that need immediate attention.
Early evaluation can help prevent complications and avoid major surgeries.
Why Choose Dr. Sumit Kapadia
As a practicing vascular and endovascular surgeon in India, I have helped thousands of patients regain mobility and avoid amputations with timely diagnosis and treatment of PVD.
At our specialized vascular care center, we offer:
- Accurate diagnosis with Doppler ultrasound and angiography
- Advanced non-surgical and surgical treatments
- Personalized lifestyle and medical management plans
- A compassionate team trained in vascular health
Our aim is not just to treat the condition but to improve the overall quality of life for our patients. Choosing the right specialist for vein can make all the difference in the outcome of your treatment.
Conclusion
Peripheral Vascular Disease is more common than most people realize, especially among those over 50 or living with diabetes or heart disease. The symptoms may seem mild at first, but can become dangerous if ignored.
The key to successful treatment lies in early detection and timely care. With the right guidance, lifestyle changes, and treatment, patients with PVD can lead active, healthy lives.
If you are experiencing leg pain, fatigue, or skin changes, do not delay in getting evaluated. As a vascular surgeon, I encourage you to prioritize your vascular health and take the first step toward better circulation and a better life.
Frequently Asked Questions (FAQs)
Most patients recover within a few hours and can resume light activities the next day. Full recovery usually takes 24 to 48 hours.
PAD pain is best managed through a combination of supervised walking, medications to improve blood flow, and lifestyle changes such as smoking cessation and weight management. In more advanced cases, minimally invasive procedures or surgery may be needed.
Walking is considered the best exercise. Structured walking programs help improve circulation and reduce pain associated with PAD. It is recommended to walk until discomfort begins, rest, and then continue walking.
Advanced PAD may present as critical limb ischemia. This includes persistent pain at rest, non-healing ulcers, and risk of gangrene. It requires immediate medical intervention to prevent limb loss.
Costs depend on the treatment method. Lifestyle and medication management may cost a few thousand rupees per month, while angioplasty or bypass surgery may range from ₹50,000 to ₹2 lakhs, depending on the hospital and severity of the disease.
Walking cannot cure PAD, but it is one of the most effective ways to manage symptoms and improve quality of life. It increases the efficiency of blood flow to muscles and reduces pain during physical activity.

Dr. Sumit Kapadia
MBBS, MS, MRCS, DNB-Fellow



