When we talk about varicose veins, most people focus on the visual aspect, those twisted, bulging ropes just beneath the skin. But the root of the problem isn’t just gravity or aging; it’s a chronic, subtle, internal battle involving inflammation.
Inflammation is the body’s natural response to injury or stress, but when it targets your veins persistently, it initiates the cycle that leads to vein dilation, valve failure, and ultimately, visible varicose veins. Understanding this link is key to effective treatment.
What Is Inflammation of a Vein (Phlebitis)?
The technical term for inflammation of a vein is phlebitis. This condition occurs when the inner lining of a vein (the endothelium) becomes inflamed.
- Causes: Phlebitis can be triggered by several factors. It might be due to direct trauma to the vein, prolonged immobility (which causes blood stagnation), or underlying systemic issues.
- Consequences: When the vein lining is inflamed, the walls can become sticky, leading to the formation of a clot (thrombus). This condition is known as thrombophlebitis. If this occurs near the surface, it’s called superficial thrombophlebitis.
How Inflammation Leads to Varicose Veins
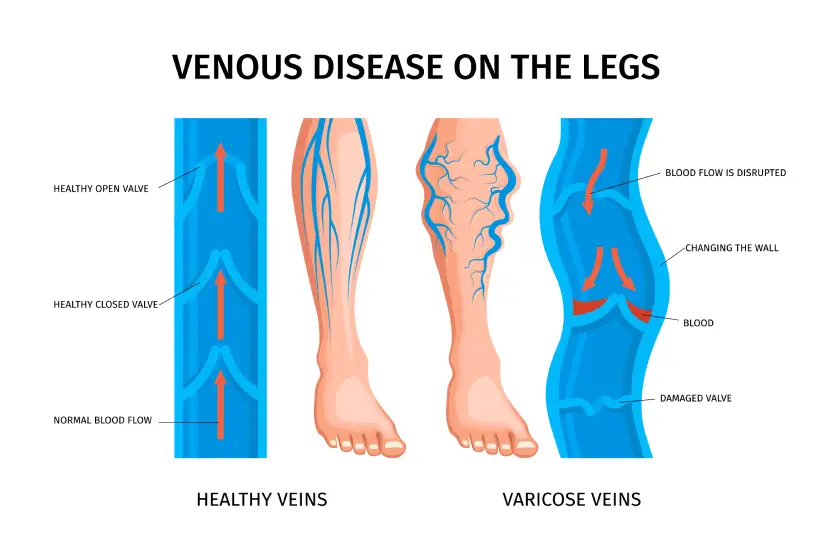
Chronic, low-grade venous inflammation legs is a primary factor in the development of varicose veins. The process looks like this:
- Endothelial Damage: Chronic high pressure inside the vein (due to factors like prolonged standing or inherited weak vein walls) causes mechanical stress on the inner lining (endothelium).
- Inflammatory Response: The damaged endothelium releases chemicals (cytokines) as part of an inflammatory reaction.
- Valve Weakening: These inflammatory chemicals actively break down the collagen and elastin that give the vein walls their strength and elasticity. This weakening extends to the tiny, one-way valves inside the vein.
- Reflux and Varicosity: Once the valves weaken and fail (venous reflux), blood pools backwards, the pressure skyrockets, and the vein stretches, swells, and becomes twisted—the visible varicose vein. This pooling itself then perpetuates further vein inflammation reasons.
Inflammation of Arteries and Veins: Key Differences
While both are vessels, inflammation of arteries and veins carries different clinical significance:
- Arterial Inflammation (Arteritis): Usually signals a more severe systemic disease (like vasculitis or accelerated atherosclerosis). It can lead to arterial narrowing (stenosis) and blockages, causing tissue death (ischemia), often seen in conditions like Peripheral Artery Disease (PAD).
- Venous Inflammation (Phlebitis): Primarily driven by blood stagnation and high pressure. Its main risk is clot formation (thrombosis). In varicose veins, the inflammation is generally chronic and low-grade, leading to structural failure.
Symptoms of Venous Inflammation in the Legs
When phlebitis is active, especially superficial thrombophlebitis, the symptoms are quite distinct from simple varicose vein discomfort:
- Pain and Tenderness: The area over the affected vein becomes painful and tender to the touch.
- Redness and Warmth: The skin directly over the inflamed segment will appear red and feel unusually warm.
- Cording: The vein itself may feel hard, like a firm cord beneath the skin.
- Swelling: Localized swelling may occur around the inflamed vein. These active symptoms signal a need for prompt medical evaluation.
When Varicose Veins Become a Medical Problem
Varicose veins often start as a cosmetic concern, but the underlying vein inflammation reasons mean they are fundamentally a progressive medical condition. They cross the line from cosmetic to medical when they cause:
- Chronic Pain and Heaviness: Persistent aching, throbbing, or a feeling of heaviness, especially after standing.
- Skin Changes: Development of skin discoloration (hyperpigmentation), scaling, or hardening (lipodermatosclerosis) near the ankles.
- Ulceration: The most severe stage, where poor circulation and inflammation lead to open, non-healing venous ulcers.
Diagnosis and Treatment Options
Diagnosis of chronic venous insufficiency (the underlying cause of varicose veins) typically involves a physical exam and a Duplex Ultrasound. This noninvasive test maps the blood flow and identifies leaky valves (reflux).
Modern varicose vein surgery and treatment options are overwhelmingly minimally invasive:
- Endovenous Laser Ablation (EVLA): The most common procedure, sealing the faulty main vein with laser energy.
- Sclerotherapy: Injecting a solution to seal smaller varicose and spider veins.
- Phlebectomy: Removing smaller varicose veins through tiny incisions.
Treating the reflux and removing the faulty vein eliminates the source of chronic pressure and reduces the ongoing inflammation.
Seeing a Varicose Vein Specialist in Vadodara
If you are experiencing pain, skin changes, or signs of phlebitis, it’s time to see a specialist. A varicose vein specialist in Vadodara, typically a vascular surgeon, is the most qualified professional to provide an accurate diagnosis and the full range of modern minimally invasive treatments.
They can assess whether your veins simply need cosmetic attention or if there is a deeper problem requiring structural repair to prevent complications like ulcers or chronic phlebitis. Seeking expertise ensures you receive personalized care for long-term relief.
Protecting Your Veins Long-Term
Preventing the triggers of chronic inflammation is key to long-term vein health.
- Maintain a healthy weight to reduce pressure on leg veins.
- Avoid prolonged periods of standing or sitting; move every 30 minutes.
- Exercise regularly, as calf muscle contractions are vital for pumping blood back to the heart.
- Wear medical-grade compression stockings, which physically support the veins and reduce swelling and inflammation.
Conclusion
The link between chronic inflammation of a vein and the development of varicose veins is clear: sustained pressure weakens the vein structure, and the resulting inflammation perpetuates the cycle of damage and valve failure. Varicose veins are not merely cosmetic; they are a sign of progressive vascular disease.
By recognizing the symptoms of venous inflammation legs and consulting with a qualified varicose vein specialist in Vadodara promptly, you can access effective, minimally invasive treatments that eliminate the source of the problem, manage the associated inflammation, and protect your venous health for years to come.
Frequently Asked Questions
The main vein inflammation reasons are high pressure within the vein (venous hypertension), blood stagnation due to immobility, and physical trauma to the vein wall. In varicose veins, the high pressure causes chronic, low-grade inflammation that damages the vein’s internal structure.
Varicose veins caused by structural valve failure and reflux cannot be cured with medication or creams. While anti-inflammatory medications can help manage the immediate pain of phlebitis, effective long-term varicose vein surgery or minimally invasive treatments (like laser ablation or sclerotherapy) are required to eliminate the faulty vein and the source of the high pressure.
To find the best vascular surgeon in India for varicose vein treatment, look for specialists who are certified and who specifically perform modern, minimally invasive procedures like EVLA (Endovenous Laser Ablation) and sclerotherapy, rather than older, more invasive stripping surgery. Experience in these advanced techniques is key to better outcomes and faster recovery.
You should worry and seek immediate medical attention if you notice signs of acute inflammation of a vein: sudden, severe pain, redness, warmth, and the feeling of a hard, palpable cord in your leg (which indicates potential superficial thrombophlebitis). This requires a rapid assessment to rule out the possibility of a deep vein thrombosis (DVT).

Dr. Sumit Kapadia
MBBS, MS, MRCS, DNB-Fellow



