Understanding Venous Disease
Venous diseases are more than just a cosmetic concern—they are medical conditions that can have significant implications for health and quality of life. These conditions, primarily affecting the veins in the legs, can range from mild discomfort to severe complications. Understanding venous diseases, including varicose veins and deep vein thrombosis, is crucial for effective management and treatment.
This comprehensive guide delves into the nature of venous disease, the types of venous diseases, their causes, symptoms, risk factors, diagnostic methods, treatment options, and the importance of consulting a specialist.
What is Venous Disease?
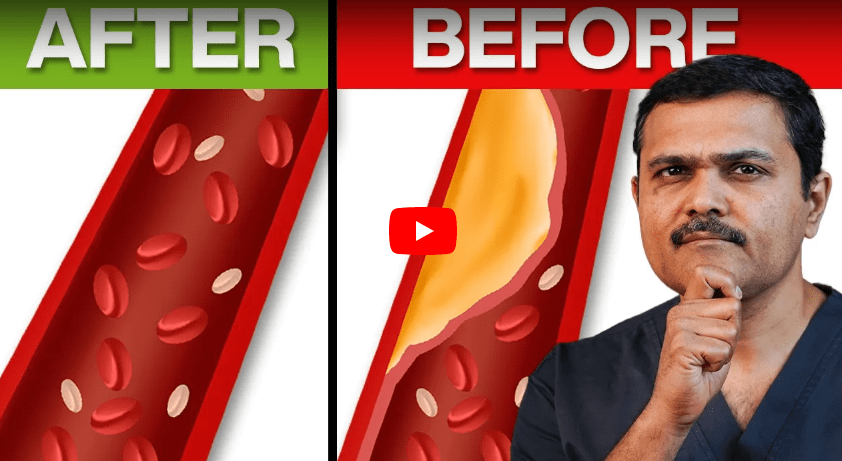
Venous disease encompasses a variety of conditions that affect the veins, primarily those in the legs. These conditions arise when the veins fail to efficiently return blood from the legs back to the heart, leading to blood pooling, increased pressure in the veins, and various symptoms. Venous diseases are widespread, affecting millions globally. They are not only a cosmetic issue but can also lead to significant medical complications if not treated appropriately.
What are the Different Types of Venous Diseases?
Venous diseases cover several conditions, each with unique characteristics and treatment needs:
- Varicose Veins: These are enlarged, twisted veins that are visible under the skin, commonly occurring in the legs. Varicose Veins are often symptomatic, causing pain, discomfort, and aesthetic concerns.
- Chronic Venous Insufficiency (CVI): This condition occurs when the veins are unable to return blood effectively to the heart, leading to symptoms such as swelling, pain, and skin changes in the legs.
- Deep Vein Thrombosis (DVT): A serious condition involving the formation of a blood clot in a deep vein, usually in the legs. DVT can lead to severe complications, including pulmonary embolism, where a clot travels to the lungs.
- Spider Veins: These are smaller, less severe than varicose veins, and appear as red or blue thread-like lines on the skin’s surface, often on the legs and face.
- Venous Leg Ulcers: Venous leg ulcers are chronic open sores or wounds that develop on the legs due to long-term poor venous return, typically around the ankles.
What Causes Venous Disease?
Venous diseases are primarily caused by the malfunction of the vein valves, which are responsible for preventing the backward flow of blood. Factors contributing to venous disease include:
- Genetic Predisposition: A family history of venous disease increases the likelihood of developing similar conditions.
- Age: As people age, their veins lose elasticity, and the valves can weaken, increasing the risk of venous disease.
- Gender: Women are more susceptible to venous diseases, likely due to hormonal changes during pregnancy, menstruation, or menopause that affect vein function.
- Obesity: Excess weight increases pressure on the veins, particularly in the legs, which can lead to vein problems.
- Pregnancy: Increased blood volume and pressure on the veins during pregnancy can contribute to venous disease.
- Prolonged Sitting or Standing: Activities that involve extended periods of immobility can impair blood flow in the veins, leading to venous insufficiency.
What are the Symptoms of Venous Disease?
The symptoms of venous disease can vary based on the specific condition but often include:
- Varicose Veins: Swollen, twisted veins that are visible under the skin, usually in the legs, causing pain, itching, or a heavy feeling.
- Chronic Venous Insufficiency: Persistent leg pain, swelling, aching, and changes in skin color and texture, particularly after long periods of standing.
- Deep Vein Thrombosis: Pain, swelling, and redness in one leg, often accompanied by warmth over the area of the clot.
- Spider Veins: Small, red or blue lines visible on the skin’s surface, typically found on the legs or face, and usually asymptomatic.
- Venous Leg Ulcers: Chronic wounds on the legs, often around the ankles, that do not heal due to poor blood flow.
Also read – Difference Between Spider Veins and Varicose Veins
Risk Factors for Venous Disease
Several factors can increase the risk of developing venous diseases:
- Family History: A genetic predisposition can increase the likelihood of vein valve dysfunction.
- Age: Older adults are at higher risk due to the natural weakening of vein walls and valves over time.
- Gender: Hormonal changes in women, particularly during pregnancy, menstruation, or menopause, can increase the risk.
- Obesity: Excess weight can put additional pressure on the veins, exacerbating vein problems.
- Sedentary Lifestyle: Lack of physical activity can lead to poor circulation and weakened vein function.
- Occupation: Jobs that require prolonged periods of standing or sitting can contribute to venous disease.
Also read – 7 Ways to Protect Your Legs from Varicose Veins at Work
How is Venous Disease Diagnosed?
Diagnosing venous disease typically involves a combination of medical history review, physical examination, and diagnostic tests:
- Physical Examination: A doctor will inspect the legs for signs of varicose veins, spider veins, swelling, and skin changes.
- Ultrasound: Doppler ultrasound is commonly used to assess blood flow and the function of vein valves, providing a clear image of the veins and the blood flow within them.
- Venography: A diagnostic imaging technique that involves injecting a contrast dye into the veins to visualize them via X-ray, used for complex cases.
- Blood Tests: These may be conducted to rule out other conditions that could be causing similar symptoms.
These diagnostic methods help healthcare providers understand the extent and severity of venous disease, guiding appropriate treatment plans.
How Can Venous Diseases Be Treated?
Treatment for venous diseases depends on the type and severity of the condition. Common treatment options include:
- Lifestyle Modifications: Regular exercise, weight management, and avoiding prolonged periods of sitting or standing can help manage symptoms.
- Compression Therapy: Wearing compression stockings can help improve blood flow in the legs, reducing symptoms of venous insufficiency.
- Sclerotherapy: A minimally invasive procedure where a solution is injected into varicose veins to cause them to collapse and fade.
- Laser Therapy: Used to treat spider veins and small varicose veins by closing them off with laser energy, offering a less invasive alternative to surgery.
- Surgical Interventions: In cases where other treatments are not effective, surgical options such as vein stripping, endovenous laser therapy (EVLT), or radiofrequency ablation may be necessary.
The choice of treatment depends on the severity of symptoms, the type of venous disease, and the patient’s overall health.
When Should You Consult a Varicose Veins Specialist?
Consulting a varicose veins specialist is advised if you experience symptoms such as persistent leg pain, swelling, skin changes, or the appearance of varicose veins or spider veins. Early consultation can lead to earlier diagnosis and treatment, preventing complications and improving outcomes. A specialist can provide personalized advice and treatment options based on the specific details of the condition.
Conclusion
Venous diseases encompass a variety of conditions affecting the veins, especially in the legs. These conditions can cause significant discomfort and lead to severe complications if not managed effectively. Understanding the types, causes, symptoms, and treatment options for venous diseases is crucial for anyone affected by these conditions.
If you suspect you have a venous disease, consulting with a qualified vein specialist can provide the necessary care and treatment to manage your condition effectively. With the right medical intervention, venous diseases can be managed, improving your health and quality of life.
FAQs
The most common cause is the weakening of the vein valves, which allows blood to flow backward and pool in the veins, causing them to swell. This are called as primary varicose veins
While varicose veins can be a cosmetic concern, they can also cause pain, discomfort, and complications such as skin ulcers or bleeding if not treated.
Treatment for DVT typically involves blood thinners, compression therapy, and in some cases, catheter-directed thrombolysis or surgery to remove the clot.
While not all venous diseases can be prevented, maintaining a healthy lifestyle, regular physical activity, and managing risk factors like obesity can reduce the risk.
You should see a doctor if you experience symptoms such as persistent leg pain, swelling, visible varicose veins, or if you have risk factors for venous disease. Early intervention can lead to better outcomes.

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.